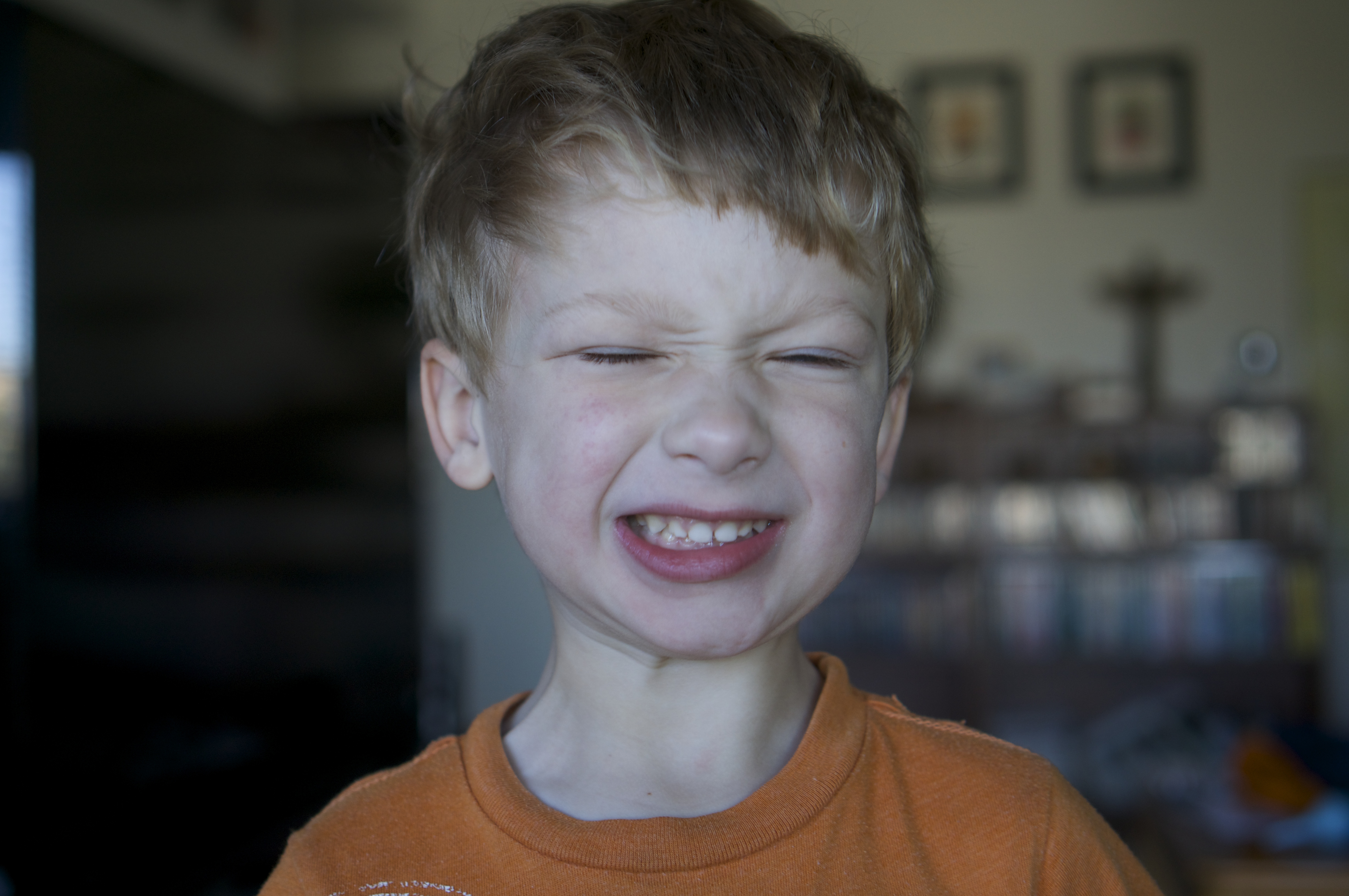
We met with our genetic councilors today, and they confirmed that Clark does in fact have Dyskeratosis Congenita (DKC). The specific version of DKC is known as TINF2, which is a marker they have identified in Clark’s DNA.
This is about where the world’s knowledge on the topic ends.
We had prepared for this visit with the genetic councilors by writing down all our questions. There were a lot. This turned out to be a waste of paper. Knowledge of this disorder spans about 10 years, and we are all learning about this in “real time”.
There is no way to tell how Clark got this disorder. It doesn’t appear to be “x-linked”, and therefore it doesn’t appear to have been passed to him from either of us. DKC doesn’t appear to come from exposure to chemicals or radiation, from what they know so far. From our knowledge today, it is simply a random bit of bad luck. One in a million. If we have another child, it will be a random chance this could happen again.
What we did learn, is that worrying about DKC in your child is like worrying about Down Syndrome. When you are told that your child has Down Syndrome, you don’t really argue that the child has the disorder, but you become very concerned about what the effects will be. Will they be able to function normally? Will it be only cosmetic? How bad will the brain damage be? etc… In all cases, doctors will tell you they aren’t sure, and that time will only tell.
DKC is identical in this scenario. Doctors know Clark has DKC, and that this can cause short telomeres, which can lead to organ failure. But what organs? When could they fail? What symptoms should we watch for? Well, there isn’t any good answers to this.
Previously, people who are born with DKC didn’t live very long. Only about 10 years ago, did we even come up with a test to identify this disorder. So there simply isn’t any good data on the subject. Clark will unfortunately be more valuable to mankind as a data point, than the reverse.
One thing that became clear in our visit with the geneticists, is that Clark’s liver, lungs and heart will be more delicate than those of a normal healthy human being. His body’s ability to maintain cellular structure of these organs is compromised. So like a muscle that repairs itself to remain strong, Clark is less likely to be able to make these repairs. When you combine this with a bone marrow transplant, the situation becomes morbid.
An otherwise healthy patient that receives a bone marrow transplant will run the risk of having liver, lung and heart conditions many years later. Pulmonary fibrosis at 50 might be one example of this. But in Clark’s case, his organs are already compromised by having DKC. So maybe it will be age 10 that Clark gets this – or maybe not. There is no way to predict any of this.
There was a sliver of positive news, in that “as far as we know…” intellectual function is not affected by DKC. With today’s information, there doesn’t appear to be any known correlation.
When it comes to how long Clark will live, or what lies ahead, it will be a waiting game to see what comes next. For “known conditions”, doctors always point to Aplastic anemia as a “worst case” scenario. Clark is already there. So would you take this as the worst is known… or a warning as to what is ahead?